Introduction
SARS-CoV-2 infection promulgates an immune dysregulation that drives an inflammatory cascade therefore inducingmorbidity and mortality across the COVID-19 presentation spectrum. Hemogram (CBC) derived traits associated with COVID-19 severity have been reported (Meizlish ML et al., 2021, Dhinata KS et al., 2021), but their relative impact across SARS-CoV-2 variants is unclear. We employed sequential machine learning approachesto identify significantly contributing traits with attendant portion of explained variance (EV%) in hospital mortality risk models across predominant SARS-CoV-2 variants.
Methods
Our retrospective design, analyses and interpretations followed constructs detailed in the Strengthening the Reporting of Observational Studies in Epidemiology reporting guideline. Adult patients with laboratory confirmed COVID-19 who underwent index hospitalization during Wuhan/D614G (March 14, 2020- June 18, 2021), Delta (June 19, 2021- December 18, 2021), Omicron (December 19-March 30, 2022) or Omicron BA.x (March 31, 2022 - April 14, 2023) variant waves at an 820-bed academic public health trust hospital in Florida were studied. Demographics, laboratory results (within 24h of presentation), ICD-10-CM-based comorbidity, COVID-19 directed treatment and administrative data were extracted from electronic medical records under IRB exemption. Generalized regression with adaptive LASSO identified hemogram-derived traits significantly associated with mortality in at least one of the variants while controlling for presentation vital signs, age, sex, extant comorbidities and ultimate COVID-19 directed treatment. Boosted Tree modeling computed within-variant proportion contributed by each trait to model's accuracy (R 2) representing EV% of mortality risk. Traits contributing to one or more variants for at least 1% portion of EV were retained in model. A Bonferroni corrected two-tailed p < .0125 was considered significant.
Results
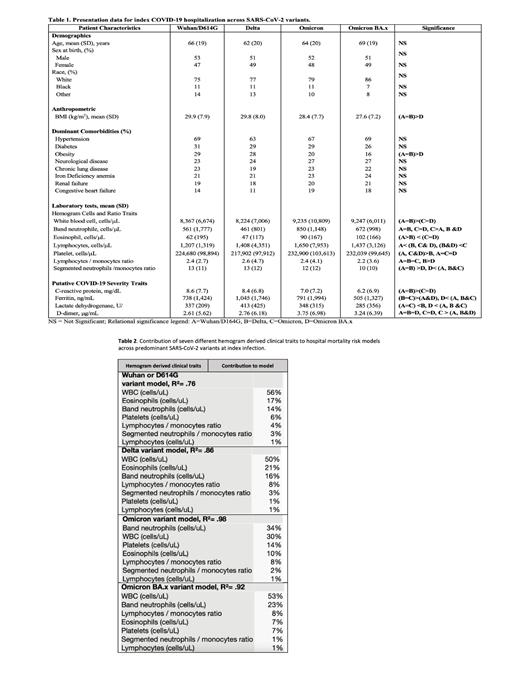
We included 6490 consecutively discharge patients distributed across Wuhan/D614G (n=2249), Delta (n=1196), Omicron (n=953) and Omicron BA.x (n=2092) variants with respective mortality of 9.3%, 13.0%, 4.4%, and 2.4% (p< .0001). Patient characteristics and on-presentation laboratory medicine clinical traits are in Table 1. Table 2 provides ranked contribution for each of the 7 traits retained in the model with attendant presentation mortality risk accuracy (R 2) across variant waves. Potent synergy can be generated with biomarkers ratios, as seen with Segmented neutrophil/monocyte ratio (SMR) and lymphocyte/monocyte ratio (LMR), compared to studying these variables individually.
Conclusion
Sequential machine-learning approaches identified differential expression intensity across SARS-CoV-2 variants in presentation hemogram-derived traits associated with hospital mortality risk modeling at index infection. These findings suggest that COVID-19 presentation risk and level of care assessment tools employing hemogram-derived traits may not generalize across pandemic variants. Platelets counts were associated with mortality in Delta, Wuhan/D614G and Omicron variants. Although it was also associated in Omicron Bx.5, the R 2 is lower, this can be explained because in this study the variant of Omicron Bx.5 had the lowest mortality rate. Studies have shown that platelet activation generates a cascade with more thromboxane A2 and platelet thrombofactor A which increases prothrombotic states (Dhinata KS et al., 2021). The absence of eosinophils was seen in Wuhan/D614G and Delta, the cause of which cannot be ascertained. A theory is that the inflammation caused by SARS-CoV-2 infection releases certain cytokines that induce eosinophil apoptosis (Dhinata KS et al., 2021). Immature neutrophils evidenced across variants can be explained by the inflammatory cascade inducing G-CSF and IL-8 production, which induces neutrophil activation (Meizlish ML et al., 2021).Lymphopenia seen throughout variants contributes to an increase in LMR. One presumption is that the SARS-CoV-2 affects T-Lymphocytes through ACE-2 receptor and CD117 spike proteins (Meizlish ML et al., 2021). Overall, our study brings to attention how hemogram-derived traits express differently across SARS-CoV-2 variants, which could guide the stratification of COVID-19 severity and assist in the care of patients before decompensation is noticed.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal